The healthcare industry is undergoing a significant transformation, driven by the shift from volume-based to value-based medicine. This paradigm change focuses on delivering high-quality care, improving patient outcomes, and reducing healthcare costs. As value-based medicine gains traction, it profoundly impacts various aspects of healthcare administration, including credentialing and contracting for medical providers and facilities. In this article, we will explore the core principles of value-based medicine and its implications for credentialing and contracting processes.
Understanding Value-Based Medicine
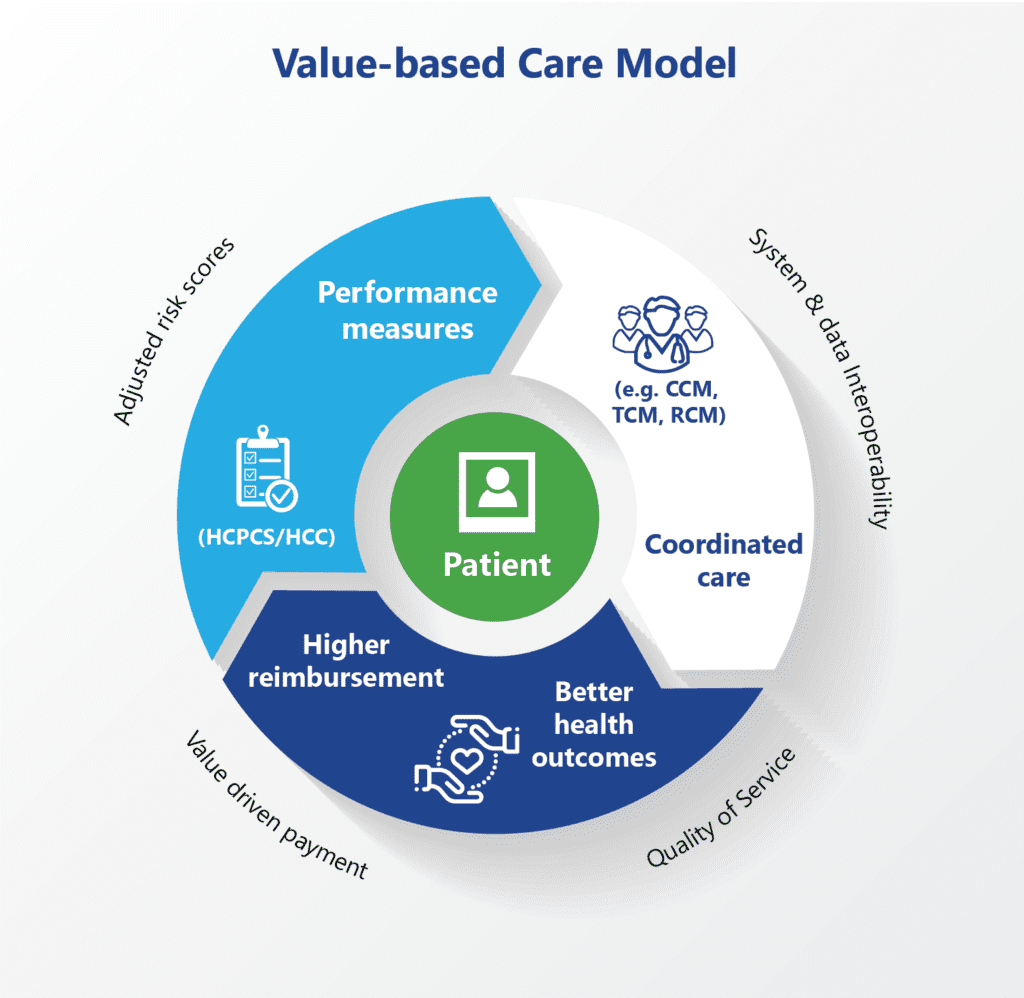
Value-based medicine emphasizes patient-centered care, where providers are rewarded for the quality of care they deliver rather than the quantity of services provided. This model aims to enhance patient outcomes, improve care coordination, and reduce unnecessary medical interventions. Key components of value-based medicine include:
- Patient Outcomes: Providers are incentivized to achieve better health outcomes for patients, focusing on preventive care and chronic disease management.
- Cost Efficiency: By reducing redundant and unnecessary procedures, value-based medicine aims to lower overall healthcare costs.
- Care Coordination: Integrated care teams work collaboratively to provide seamless and efficient care across various settings.
Impact on Credentialing
Credentialing is the process of verifying the qualifications and professional background of healthcare providers. In a value-based system, credentialing processes must adapt to emphasize quality and outcomes over sheer volume. Here’s how value-based medicine impacts credentialing:
- Enhanced Quality Metrics: Credentialing bodies are now prioritizing quality metrics, such as patient satisfaction scores, readmission rates, and clinical outcomes. Providers are assessed based on their ability to deliver high-quality care consistently.
- Continuous Education and Training: To stay aligned with value-based care principles, providers must engage in ongoing education and training. Credentialing processes now incorporate continuous learning requirements to ensure providers are up-to-date with the latest best practices and technologies.
- Interdisciplinary Collaboration: Value-based care encourages teamwork and collaboration. Credentialing now often requires verification of providers’ experience in multidisciplinary team settings, ensuring they can effectively contribute to coordinated care efforts.
- Technological Proficiency: Providers need to be proficient with health information technology (HIT) systems, such as electronic health records (EHRs) and data analytics tools. Credentialing processes are evolving to include assessments of technological competence.
Impact on Payer Contracting
Contracting in healthcare involves establishing agreements between providers, facilities, and insurance companies(payers). The shift to value-based medicine necessitates changes in how these contracts are structured and managed:
- Outcome-Based Contracts: Traditional fee-for-service contracts are being replaced by outcome-based contracts. These agreements tie reimbursement to the achievement of specific health outcomes, incentivizing providers to deliver quality care efficiently.
- Shared Risk and Rewards: Value-based contracts often include provisions for shared risk and rewards. Providers and payers share the financial risks associated with patient care, but they also share in the savings generated by improved health outcomes and cost reductions.
- Performance Metrics: Contracts now incorporate detailed performance metrics that align with value-based care goals. Providers must meet specified benchmarks related to patient outcomes, cost savings, and care quality to receive full reimbursement.
- Flexibility and Adaptability: Value-based contracts are designed to be more flexible and adaptive to changing healthcare landscapes. This adaptability ensures that contracts remain relevant and effective as new value-based care initiatives and technologies emerge.
- Focus on Population Health: Contracts are increasingly focusing on population health management, encouraging providers to address the health needs of entire patient populations rather than individual patients. This holistic approach promotes preventive care and chronic disease management.
Challenges and Opportunities
The transition to value-based medicine presents both challenges and opportunities for credentialing and contracting:
- Data Integration: Effective implementation of value-based care requires robust data integration across various health information systems. Ensuring accurate and timely data exchange is crucial for tracking performance metrics and outcomes.
- Standardization: Developing standardized criteria for quality metrics and performance benchmarks is essential for consistency in credentialing and contracting processes.
- Collaboration: Greater collaboration between providers, payers, and regulatory bodies is necessary to align incentives and achieve common goals in value-based care.
- Patient Engagement: Engaging patients in their care journey and encouraging adherence to treatment plans are critical for the success of value-based initiatives.
Conclusion
Value-based medicine is transforming the healthcare landscape, with significant implications for credentialing and contracting processes. By focusing on quality, outcomes, and cost efficiency, value-based care promotes a more sustainable and patient-centered healthcare system. As credentialing and contracting adapt to this new paradigm, providers and facilities must embrace continuous improvement and collaboration to thrive in a value-based world. Through these efforts, the ultimate goal of delivering high-quality, affordable care to patients can be achieved.