When it comes to running a successful medical practice, the importance of insurance enrollment and credentialing can’t be overstated. It’s one of those behind-the-scenes tasks that, if done well, ensures you get paid on time and can focus on patient care. But let’s be honest—navigating the maze of insurance networks, credentialing processes, and provider enrollment can be a nightmare. So, how do you choose the right partner to handle this crucial aspect of your practice? Here are the top five things to consider when evaluating service partners for insurance enrollment and credentialing.
1. Experience and Expertise
First and foremost, you want a partner who knows the ropes. Credentialing and insurance enrollment are complex fields that require in-depth knowledge and expertise. Look for a company that has been in the business for a significant amount of time and has a proven track record. Experienced providers are more likely to understand the nuances of different insurance companies and state-specific requirements, which means they can navigate the process more efficiently.
When evaluating potential partners, ask about their history and the experience level of their staff. A team with a solid background in provider enrollment and credentialing will be able to anticipate and resolve issues before they become major problems. They’ll also be better equipped to handle unique situations that may arise, such as credentialing for specialized providers or dealing with multiple insurance networks.
2. Comprehensive Services
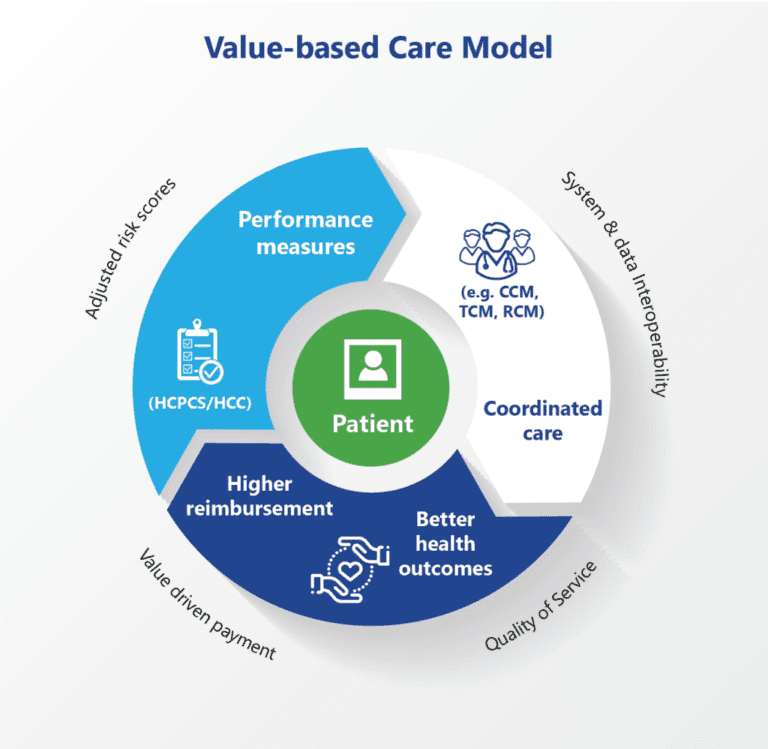
Insurance enrollment and credentialing encompass a wide range of tasks, from initial application submissions to ongoing re-credentialing and contract negotiations. A good partner should offer comprehensive services that cover every aspect of the process. This includes everything from verifying provider information and preparing applications to following up with insurance companies and handling denials or appeals.
Make sure to inquire about the full scope of services offered. The more comprehensive the service, the less you’ll have to worry about. This can save your practice a significant amount of time and effort, allowing you to focus on what matters most—providing excellent patient care.
3. Customization and Flexibility
No two medical practices are exactly alike, so a one-size-fits-all approach to provider enrollment and credentialing won’t cut it. Look for a partner who can tailor their services to meet your specific needs. This means they should be willing to understand your practice’s unique requirements and adapt their processes accordingly.
Customization might involve creating a personalized credentialing plan for your practice, providing specialized support for particular providers, or even integrating their services with your existing practice management system. Flexibility is key—your partner should be able to scale their services as your practice grows and changes.
4. Communication and Transparency
Good communication is essential in any partnership, but it’s especially important when it comes to provider enrollment and credentialing. The process involves a lot of back-and-forth with insurance companies and other stakeholders, so you need a partner who keeps you in the loop every step of the way.
Ask potential partners about their communication practices. How often will they update you on the status of your applications? Do they provide a dedicated account manager or a single point of contact? Transparency is equally important—your partner should be upfront about their processes, timelines, and any potential issues that might arise. Clear, open communication ensures that you’re never left in the dark about the status of your credentialing and enrollment efforts.
5. Customer Support and Service
Last but certainly not least, consider the level of customer support and service provided. Credentialing and insurance enrollment can be stressful, and you need a partner who is responsive and available to address your concerns. Excellent customer service can make a world of difference, turning a potentially frustrating experience into a smooth and manageable one.
Look for a partner who offers robust customer support, including easy access to support staff, timely responses to inquiries, and a commitment to resolving issues quickly. Read reviews or ask for references to get a sense of their customer service reputation. A partner who prioritizes your satisfaction is more likely to go above and beyond to ensure your needs are met.
Wrapping It Up
Choosing the right partner for insurance enrollment and credentialing is a critical decision that can significantly impact your practice’s efficiency and financial health. By focusing on experience and expertise, comprehensive services, customization and flexibility, communication and transparency, and customer support and service, you can find a partner who will help streamline these complex processes and allow you to focus on delivering top-notch patient care.
Remember, the goal is to find a partner who understands the intricacies of provider enrollment and can provide the support you need to navigate this challenging landscape. Take your time, do your research, and don’t be afraid to ask tough questions. Your practice—and your peace of mind—deserve nothing less.
So, when you’re ready to make the leap, keep these five key factors in mind. With the right partner by your side, insurance enrollment and credentialing can become a seamless part of your practice’s operations, rather than a constant source of frustration. Happy hunting!